Myopathies are hereditary diseases, which are based on the muscle fiber damage and, as a consequence, the emergence of a progressive musclular dystrophy (atrophy).
Muscular dystrophy arises from the disruption of biochemical processes in the muscle fiber itself: the synthesis of nucleic acids changes, the catabolism of proteins accelerates, the content of creatine phosphokinase increases, and the level of ATP (adenosine triphosphate) decreases. Some scientists hold a theory of “defective membranes”, which is based on the loss of enzymes and amino acids by muscle fibers because of the so-called “defects” of cellular structures.
The myopathy is characterized by replacing of a part of muscle fibers by fat tissue; the muscles themselves are thinned.
There distinguish primary myopathies (which gradually develop yet in childhood and adolescence) and acquired ones. Clinical appearances of myopathy can be intensified under the influence of unfavorable procatarxis factors (infections, intoxications, nervous breakdowns).
Symptoms of myopathy
This disease begins with a gradually increasing musclular weakness in certain muscle groups. The primary proximal muscle sets (muscles of the pelvic and shoulder girdles, proximal parts of the upper and lower extremities, trunk) predominate in the majority of cases. The distal muscle groups’ damage is observed in rare and severe cases.
The symmetrical bilateral amiatrophy, hyporeflexia (decrease of tendon reflexes), hypotonus (tendon reflex decrease) develop later. On latter myopathy stages, the deformation of bones and joints develops and vegetal trophecies are clearly expressed. The joint range of motions can be either high or low (due to the shortening of the muscles and their tendons).
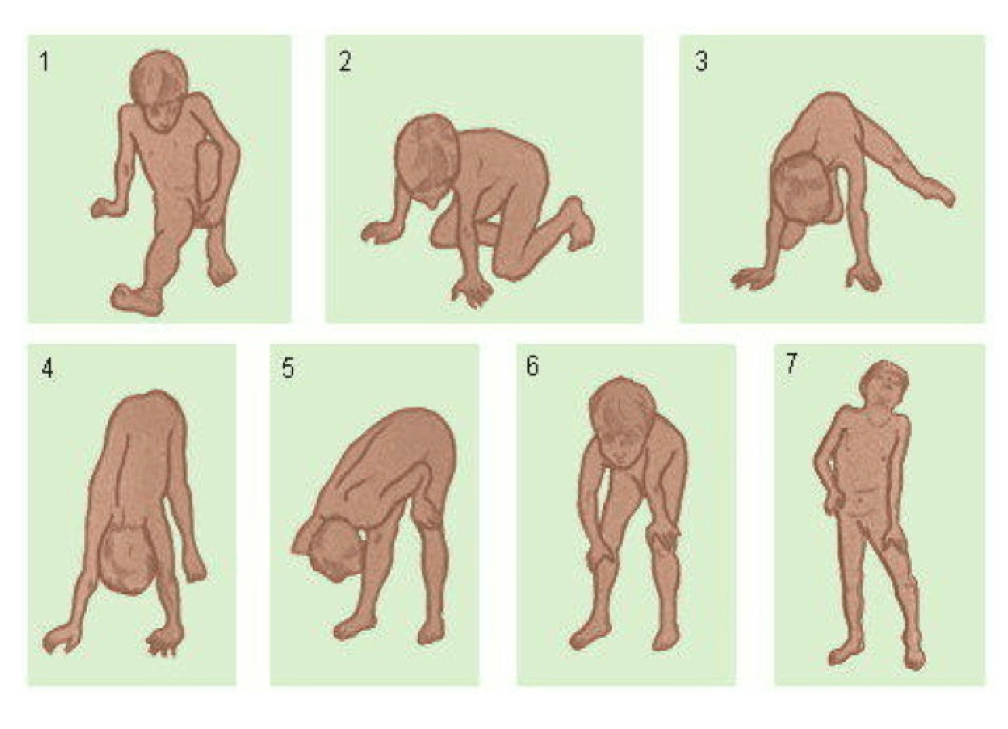
Progressing muscular dystrophy. Getting up by “Ladder” method.
The development of muscular pseudohypertrophy or “imaginary” hypertrophy is observed – a compensatory muscle expansion due to the fat and connective tissue growth. Such muscles are visually enlarged, firm, but not strong.
The most common forms of muscular dystrophy:
- Duchenne’s muscular dystrophy
This is the most common and severe muscular disease that occurs only in boys. Children inherit the pathological gene from their mother. The genetic nature of disease was proved soon after this form was first described by neuropathologist Duchenne in 1868. The dystrophin protein deficiency is at the vey core of the development of this type of muscular dystrophy.
This disease manifests itself in the first years of a child’s life with a lag in motor development, an increasing weakness of the proximal muscles of the lower limbs and pelvis. Subsequently, the process extends to the muscles of the shoulder girdle and back, at the later stages – to the muscles of the upper extremities and the respiratory muscles, i.e. by an ascending type.
Distinguishing diagnostic signs of Duchenne myopathy are pseudohypertrophy of gastrocnemius muscles and inevitable myocardial lesion. This form is characterized by contractures in the joints, curvature of the spine and thorax, foot deformity, early child’s disability. Some patients have a delay in mental development.
- Becker’s muscle dystrophy
This lighter version of myodystrophy is also transmitted to the son from the mother. The disease was first described in 1955 by neuropathologist Becker. Pathology does not develop as rapidly as Duchenne’s myodystrophy, and the first clinical symptoms can appear within teenage or adolescent years. At the heart of the disease is not the complete absence of dystrophin protein, but its defect or deficiency. Intellect of children does not suffer; development of contractures and pseudo-hypertrophies is possible.
- Erb’s juvenile myodystrophy
It was first described by neurosurgeon Erb in 1844. This disease manifests itself in teenage years (14-16 years) with the growing muscles weakness of the hips and pelvic girdle. As a result, the gait changes, resembling a “duck gait”. At the beginning, after a night’s sleep, muscle strength can be restored. Later on, practically all the body muscles are involved in the process, they become thinner, their tone decreases; the kyphosis, scoliosis, lordosis develop. However mental development does not suffer.
Progressive muscular dystrophy was considered as an absolutely incurable disease in the past. Now there are a number of therapeutic methods possible to stop the disease development and to achieve an improvement.
The success depends on how timely the disease is recognized and the therapy started; the last mentioned should be carried out systematically, according to a certain algorithm, taking into account the peculiarities of the current clinical form.
Early diagnosis is extremely important, as the disease progresses the muscle tissue is replaced by adipose tissue, and at the age of 14–15 years, adipocytes are detected instead of muscle cells. Timely treatment makes it possible to prolong the duration of functional activity of the child and delay the secondary skeletal changes development.
As of today, physicians have two drugs approved for the treatment of Duchenne muscular dystrophy, namely, ataluren and eteplirsen, which can only be used for certain types of mutations.
Duchenne myopathy treatment protocol also includes corticosteroids such as prednisolone and deflazacort to reduce muscle inflammation and stimulate repair.
In Bersenev’s Medical Center good results have been obtained with the metameric medicinal treatment that affect metabolism processes and improve neuromuscular conductivity (ATP, B, E vitamins, Prozerine, Neuromidin, Cerebrolysin, etc.)
Non-drug treatment:
- Moderate physical activity is recommended, swimming is allowed. Inaction (e.g. bed rest) may increase disease progression;
- Physiotherapy is important to maintain muscle strength, flexibility and joint function.
- The use of orthopedic devices can improve the patient’s ability to move and provide for their own needs.
- The use of orthoses that fix the shin during sleep allows delaying the onset of contractures (restriction of joint movements).
- As the disease progresses, it becomes necessary to use special respiratory mechanisms that allow to ensure normal process of respiration.
To make an appointment for a consultation or a treatment session, please, call +38 (044) 238-22-31 (call centre).













